It is a while since I have written a blog and that’s partly due to being busy with our new home, meeting new people, partly a lack of ‘inspiration’. Prompted by a note from Dr Michael Ward of Swansea University, who setup the CoronaDiaries Project of which mine is part, I did think about doing one more blog about the pandemic. The two-year anniversary of my first blog seemed a good time to revisit the topic. However, events of the 5th of March 2022 prevented me from writing that blog and are the inspiration for this one.
The simplest way to start is to reproduce the ‘incident report’ sent by Mark, one of the Run Directors (RD) of Delamere Parkrun, which I ran on that never-to-be-forgotten Saturday morning….
Ian Skaife collapsed around 1.2 miles into today’s run at around 9:15. He was immediately attended to by the following: June who was just in front of Ian and heard him fall, June’s partner Matthew, Nikki who was a little behind but did not see him fall. Nikki is a medical nurse (an unknown passing runner, not in Parkrun, who was also a doctor was in attendance and stayed until the paramedics arrived).
Around this time an unknown person called an ambulance.
Nikki reported there was no pulse and Ian was not breathing. Between herself and June and advice from the unknown doctor, they opened his airway and administered CPR for perhaps the next 15 minutes or so. Ian occasionally restarted breathing for a short while, but Nikki did not detect a pulse at any time she checked for one.
Shortly after the incident, perhaps at 9.20 the tail-walker (Liz) arrived who called the RD Andy. I was standing next to Andy when he received the call. At 9:22 I made a call to the Forestry Commission(FC) office. They collect the AED (Automatic External Defibrillator) and drove to the incident – the main FC contact on the day was Liam at Forestry England. I left on foot to the incident and was joined by marshal Katherine who is a medical doctor.
The FC team arrived at the incident at around 9:30 and on arrival immediately deployed the AED once. This was successful in initiating a pulse. Very shortly afterwards the paramedics arrived by which time Ian was conscious and had achieved some sort of satisfactory stability.
I arrived at the scene around 9:37 and called Ian’s ICE (In Case of Emergency number) from his wristband at 9:39. The ICE is his wife Alyson Skaife who informed me Ian was with his son, Mike Skaife (now at the finish), who Alyson then called. Mike appeared at the incident perhaps within 10 minutes.
By 9:50 Ian was on a stretcher, breathing himself and able to talk and knew where he was. The paramedics had been joined by air ambulance paramedics, though the helicopter had to land around a mile away (as we are in a forest).
At around 10:10 Ian left the immediate area in an ambulance to be taken to the helicopter which left with Ian around 10:25 for Stoke Trauma Unit.
Even now as I read the report it almost brings me to tears. I have no memory of the day other than arriving at Delamere and parking the car. I made it to the start where I met up with my son Michael. I can remember talking to a Crusader, a lady with a Superman top wearing a blue tutu and a couple of nuns! Alyson had to tell the nurse in A&E that I wasn’t hallucinating as the run was fancy dress to celebrate the 9th anniversary of Delamere Parkrun’s first event.
Mike had helped the paramedics get me into the air ambulance – apparently an older lady was nearly blown over after not getting out of the way as the helicopter took off from the crossroads where the traffic had been stopped. Alyson had been working at a pharmacy in Gobowen when she got the call from Mark and left immediately and drove to Mike’s in Northwich where they drove together to Stoke. It was the second time in almost 10 years that Alyson & Mike had sat in the family area of the hospital waiting to see if I made it. For those who don’t know what happened in 2012 you can read my blog from 2019.
https://skatchat.wordpress.com/2019/10/06/the-long-story/
I am relying on what Alyson & Mike have told me happened after leaving in the air ambulance as my next memory is waking up on Sunday morning in the Cardiac Care Unit (CCU). The junior doctor had written me a note telling me that I was in Stoke and they diagnosed that my heart stopped due to blocked artery and they had started me on some more medication. Alyson had written on the end of the note ‘Middlesbrough won 2-0’!
Back to A&E ‘Resus’ where I kept saying ‘Did I come in a helicopter? and Mike answered yes and I said ‘What a shame I missed that’. Over and over again! They decided to scan my brain for a head injury, but the image hadn’t changed since my last one in 2013. Alyson was pleased that I hadn’t been running in Oswestry as a) the defibrillator is not as close (note 9 April 2022 – having volunteered there yesterday I know this is not true as there is a portable one at the start), b) the ambulance service in rural Shropshire is not as responsive and c) they might have taken me to Shrewsbury Hospital which, although I wouldn’t have been in the recently sanctioned maternity unit, doesn’t have a good reputation. If they didn’t have my scan from 2012-13 goodness what they would have made of my slightly mushed brain!
Stoke is also where I had been diagnosed with angina in early 2021 so they were aware of that. I had been signed off after a ‘stress test’ in July when I went on the treadmill wired to an Electrocardiogram (ECG). Although I was due to have another test this coming July, as one of the A&E doctors remarked I had done my own stress test and failed spectacularly.
Alyson & Mike stayed with me until early evening and weren’t offered any drinks or food and didn’t want to leave me in case another doctor came with information. Eventually I was admitted to CCU and they sat with me there a while.

CCU is a ward of bays in a circle around a central nurses station. It is not a quiet place as we were all wired to heart monitors with electrodes attached to several sticky pads over our chests reporting to a central screen. Alarms were going off each time a lead came loose, and I was confused as I thought it was mine that was setting them off, so would try not to move. Also on my chest were two large sticky pads from the defibrillator used in the forest. The device made sleeping difficult but I was grateful just to be there. Alyson visited me later in the day and I started to learn more about what had happened.
Alyson and Michael had gone back for my car on Sunday morning as it was still parked at Delamere. Alyson parked outside the administration offices and saw Liam who had taken the AED and he was pleased to hear how well I was doing. He admitted than when he first got there and saw the medics working on me he didn’t think the ending would be good. Alyson thanked him on behalf of all of us, and only this week I emailed him to tell him how well I am doing. Often people who help others never find out what the outcome is, and that is a shame.
Alyson visited me later that day and brought my phone in so I was able to message friends and work colleagues to tell them what had happened to me. Mike was frustrated that only Alyson was allowed to visit me due to Covid-19 restrictions, and our other son David – who had been rowing with his club in Bath and left ready to come up when Alyson called him on the Saturday morning – had to make do with a Zoom update on the Sunday evening. Since the pandemic started we had been having a weekly call often with a short family quiz. I may have been able to join on my phone that evening, but was very tired and sore.
The soreness was something that, when the nurses asked me how I was feeling, I told them I was grateful for. It showed that Nikki, June and Matt and the unknown doctor had done a good job. A few weeks previously Alyson had attended a CPR and defibrillator use course, and told me that it was physically hard, and not something one person could do for more than a few minutes. Alyson had also text June & Nikki to thank them for what they had done. I sent an email to the ‘Core Team’ of volunteers at Delamere who I know well having volunteered there many times over the years. These ‘Hi-Viz Heroes’ as we call them in the Parkrun family are the reason events are free every week. I told them in the message that I was well and thanked them for what they had done.
On Monday Alyson came over in the afternoon but didn’t get to see me for long as I was taken down to what is called ‘The Lab’ to have a stent fitted. This was something that I had been due to have last July, but they decided my blood vessels were ‘perfect’. This time the situation had changed, so it was a case of putting one in to be sure. As it turned out my temperature was too high, so I was back on the ward after Alyson had left.
The next morning my temperature was fine and my bloods were ok, so I was back in the lab and this time the stent fitting was successful. As Dr Gunning my consultant said ‘that’s the plumbing sorted, all we need to do now is find a good electrician to sort you out…’. Alyson visited me later in the afternoon after tutoring pharmacy students at nearby Keele University. After getting up at 5am to travel there she said the work kept her busy, and took her mind off what was happening to me. She had also been very busy, as people often are when someone is in hospital, having to phone family and friends and taking calls from people asking how I was doing.
The ‘electrician’ turned out to be Dr Baynham who came to see me when Alyson visited on Wednesday, by which time I had been moved to a nicer room on a nearby ward. The room had been a ‘day room’ before the pandemic where patients could sit and watch TV and had panoramic views overlooking the helicopter landing site. It was converted to a 3-bed bay and was light and comfortable.

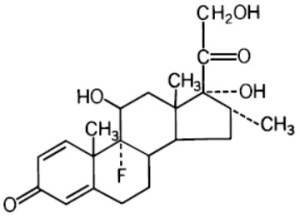
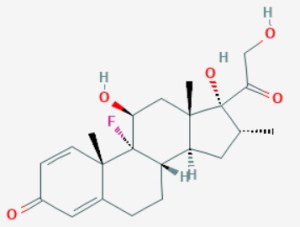
Dr Baynham said the plan was to give me an implantable cardioverter defibrillator (ICD) which would deliver a shock should my heart fail again. There were possible side effects such as infection, and it giving me a ‘shock’ when it wasn’t needed, but overall it seemed a good solution to my issue. I needed an app on my phone to send data from the ICD back to Stoke – Alyson was disappointed that it wouldn’t allow her to turn me off and on.
The procedure was planned for Friday afternoon confirmed at the ward round Friday morning. The device was fitted at about 3pm under a local anaesthetic. Due to the blood thinners I was on the surgeons struggled to get it under my collar bone in a ‘pocket’ they cut into my chest muscle, but eventually they managed. An X-Ray about two hours later confirmed it was in place with wires to my heart, and by 8pm my discharge letter and medicines were ready. Alyson came to pick me up and drove me home for 10pm. I slept in my own bed.
For the first few days home I was very sore and couldn’t sleep well on either side. This was both from the bruising to my chest and ribs from the CPR and the scar and the device under my left shoulder. I was also very weary from the whole thing, and this added to my ‘usual’ fatigue from the brain injury. I often have a short 40-minute nap during the day, but now needed one morning and afternoon. But it felt great to be home with Alyson.

The NHS had done an amazing job in the 5 days since I was admitted. I underwent two procedures, and the surgeon told me the ICD cost £30,000 (not sure if that is the cost of the device only or for the surgeons, operating theatre and nursing care). The care of all the nurses, doctors, pharmacists, physios, catering and cleaning teams was fantastic.
I sent WhatsApps to June and Nikki from Parkrun telling them that I was home and what had been done to me. I also said I was very grateful for the pain I had in my chest which showed that they did a great job! I said that without them I am certain that Alyson, Michael & David would be planning my funeral. Both sent gracious replies and June said although it was her slowest time for a Parkrun as they all took an hour and 14 minutes by the time they got back to the finish, ‘it would always be a personal best (PB) for a different reason..’ It had only been her 3rd run, and she nearly didn’t go, as it is her partner Matt who was the runner. I said that I hope that what happened wouldn’t put her off doing another!
The following weekend we had planned a trip to some cottages outside Scarborough in the north east where we have been many times. I felt strong enough to make the journey but as I can’t drive for 6 months Alyson had to do it all in our new all-electric car (the story of ‘range anxiety’ is for another blog!). We had planned to do the Parkrun at Whitby (Alyson is also a member of the ‘Parkrun Family, having done 35 since she took it up a couple of weeks before her 59th birthday). So at 9am on a Saturday two weeks after my incident the RD gave the usual pre-race briefing and when she mentioned that they had a defibrillator people start to laugh. Alyson shouted ‘It’s not funny! My husband needed one two weeks ago at a Parkrun!’ It went quiet and someone asked ‘Is he ok?‘ to which she replied ‘Yes, he’s over there watching the start..’.
Alyson enjoyed the run which was down a disused railway but reflected afterwards that the surface was hard paving, much less forgiving than the forest track at Delamere.
Last weekend we were also away at a large house with 18 of Alyson’s family and on Saturday morning a group of six went to Ross on Wye Parkrun. Five to run and me to watch. Alyson and Mike both ran in this one. However, this time no one laughed when the RD mentioned that they had one portable defibrillator at the start, and another was in the nearby sports centre. I was chatting to some other ‘tourists’ at the start, and one older guy from Leeds who, when he asked if I was running and I told him my story, announced ‘Oh I had one fitted 12 years ago and have run lots of times since including a few marathons.’
I have been told that I should be able to resume ‘normal exercise’ eventually, but am not sure I will ever do a marathon given the furthest I have ever run is several half-marathons and the last of those was the 2006 Great North Run! However, it gave me some hope.
I am not sure Alyson feels the same, but I have promised that I won’t go out on my own – as I had thought of doing the week before my incident when I fancied a quick jog up to the woods in our local area…
The final ‘twist’ to the story is that this weekend we celebrate our 40th wedding anniversary. We had booked a trip back to Paris to stay in the same hotel in the Place de La Sorbonne down from Notre Dame, where we went for our honeymoon and revisited on our 25th. There is a Parkrun close by and we had planned to do that one…it doesn’t bear thinking about what it would have been like if I suffered my cardiac arrest there – not with two failed O-Levels in French between us!
Something that Nikki replied after I shared the blog about my brain injury has stuck with me. She wrote ‘What an amazing story! I think someone up there is looking down on you!’ Another friend wrote ‘You know my thoughts on God, but you are a special case so I will pray for you’. A university friend who I will call Speed wrote ‘God clearly still has work for you to do! Thank God for all the prompt medical help you got.’
Even Alyson and her sister, neither of whom attend any church, in talking together when we were away in Ross on Wye concluded that God really didn’t want me joining him just now as that is twice I have tried and twice he has sent me back!
Since we moved from Crewe, a year ago this week, where I had been deeply involved at my local Methodist church and held various roles at circuit, district and attended the annual Methodist Conference, I have not found my ‘place’ in Oswestry. This is partly a deliberate choice as I wanted to take some ‘time out’ to discover the area and people. In September I met our local minister Rev Julia in her manse garden for a long chat. She was wonderful and encouraged me to work out what I wanted to do. This despite being very busy with pastoral care of 23 churches and knowing that, as in all places Methodist, there is a shortage of willing and experienced people for all the roles. The local churches have been very welcoming, despite numbers being down and attendance less during Covid. I have certainly not been to many services or joined local house/prayer groups, and even my attendance at the online Methodist Central Hall Westminster (MCHW) setup during ‘lockdown’ has been patchy.
Perhaps I am being given a ‘message’ through what has happened, and I definitely have more time to think things over, as I can’t just take myself out in my car without Alyson coming with me. I attended our annual ‘Covenant Service’ in January at which Methodists say a prayer which has these lines in it.
Your will, not mine be done in all things, wherever you may place me, in all that i do and in all that I may endure.
The Methodist Worship Book P.288 (Modern Form)
When there is work for me, and when there is none: When I am troubled and when I am at peace. Your will be done.
When I am disregarded: when I find fulfilment and when it is lacking;
The more traditional version is even more ‘stark’ with the lines ‘…Put me to doing, put me to suffering; let me be employed for you or laid aside for you..’
With all the cards. messages, calls and support I have had, I certainly don’t feel disregarded – quite the opposite. But in this season of Lent as we look towards the suffering of our Saviour Jesus on the cross, even though I am not doing a formal lent study, maybe I need to take some time to consider my place in the local area, my family and church, and commit to doing something positive.

I am definitely going to sign up for a CPR course and use myself as a living example of what can be done. I will commit to raising some funds or donating to any Parkruns who need to get a defibrillator. But beyond that I will try to find something in the coming months or years to take the place of the work I have done in the past for my local church and community.
I will continue to volunteer at Parkrun events and be a ‘Tail Walker’ who follows the slowest person so that no one ever finishes last. To be fair to the core Team at Delamere it might be some time before I turn up in my new branded orange Parkrun shirt – my old one having been sliced down the middle by the paramedics! And I will definitely update my ICE barcode wristband which currently says ‘ no medical conditions’!